Regenerative medicine is a new form of medicine that uses artificially processed and cultured cells or tissues to repair, regenerate, and restore certain tissue or organ functions that have been lost due to causes such as illness, accidents, or aging.
Many conditions considered hard to treat or believed to lack effective treatments (e.g., restoring brain functions of patients that have suffered brain damage from ischemic stroke, or motor functions of patients that have lost the use of their legs due to spinal cord injuries sustained in an accident) are expected to be overcome by the power of regenerative medicine in the future.
Regenerative medicine mainly uses human cells to repair and restore functions of tissues and organs. It encompasses a wide range of treatment techniques and approaches ranging from the use of microscopic cells to organ transplants.
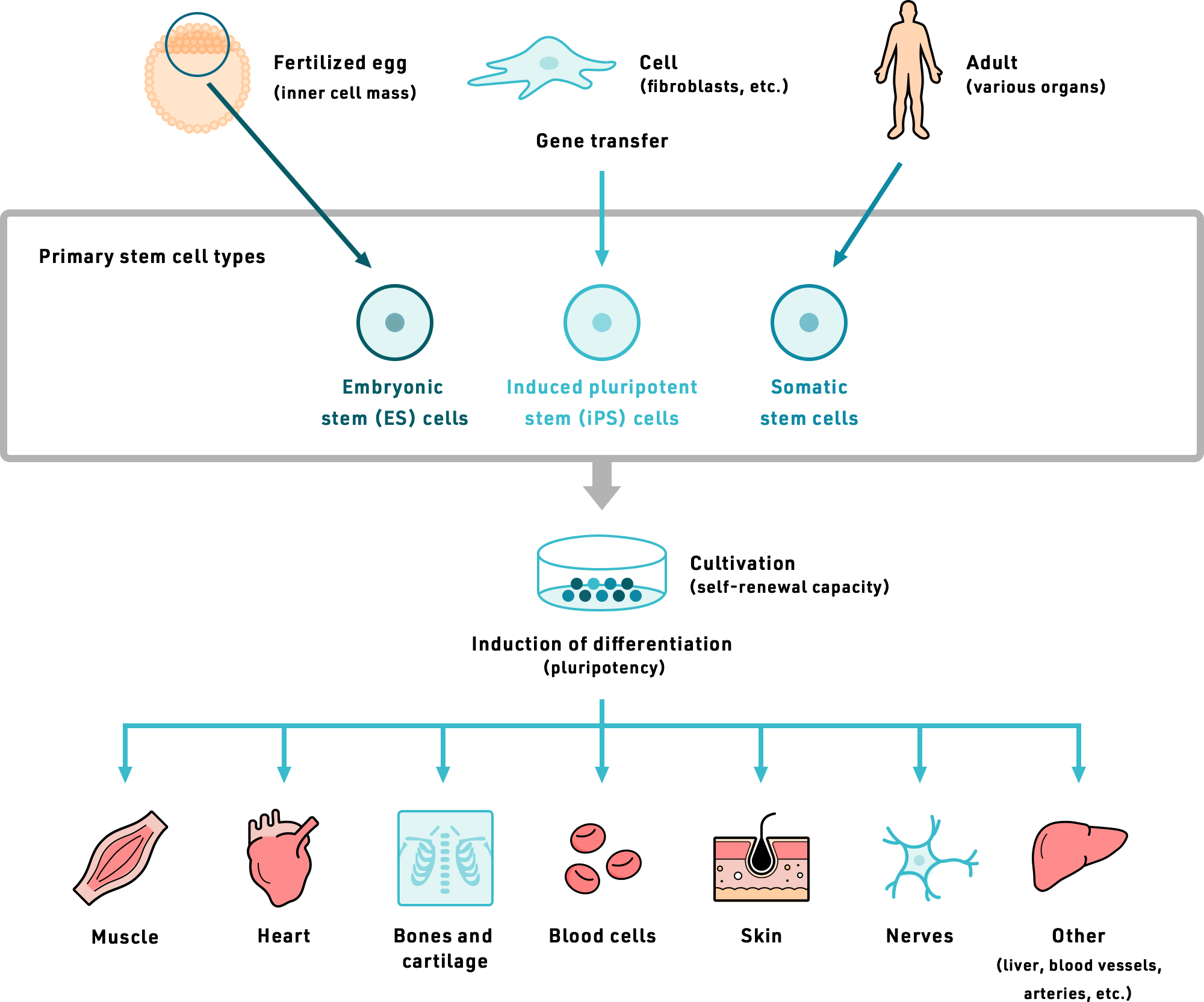
The primary cells currently being researched for applications in regenerative medicines are somatic stem cells, embryonic stem (ES) cells, and induced pluripotent stem (iPS) cells. Stem cells can differentiate or proliferate into different types of cells, and are believed to be effective in promoting repair and regeneration of tissues or organs that have been damaged due to illness or other causes. Research on regenerative medicine using cells has been underway even before iPS cells were developed.
Professor Shinya Yamanaka, who pioneered iPS cell research, won the Nobel Prize in Physiology or Medicine for his accomplishments in 2012, paving the way for widespread research in regenerative medicine around the world. The Japanese government designated regenerative medicine as a growth industry with the enforcement of the Act on Securing Safety of Regenerative Medicine and the revised Pharmaceutical Act in 2014, marking the start of a countrywide effort to lead the world in the practical application of regenerative medicines.
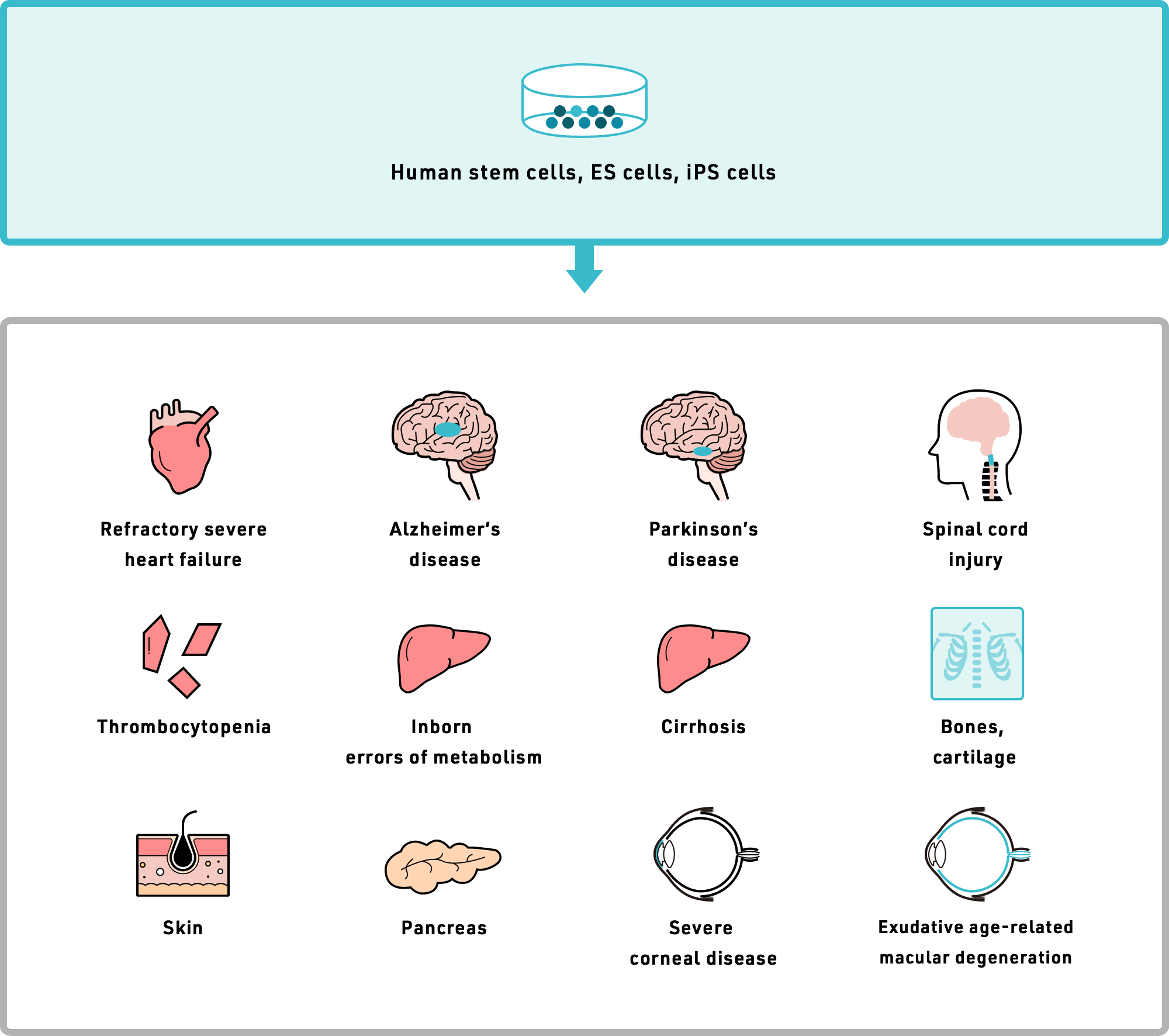
Various transplants that use cell types created from human stem cells, embryonic stem (ES) cells, or induced pluripotent stem cells (iPS) cells are being planned in Japan.
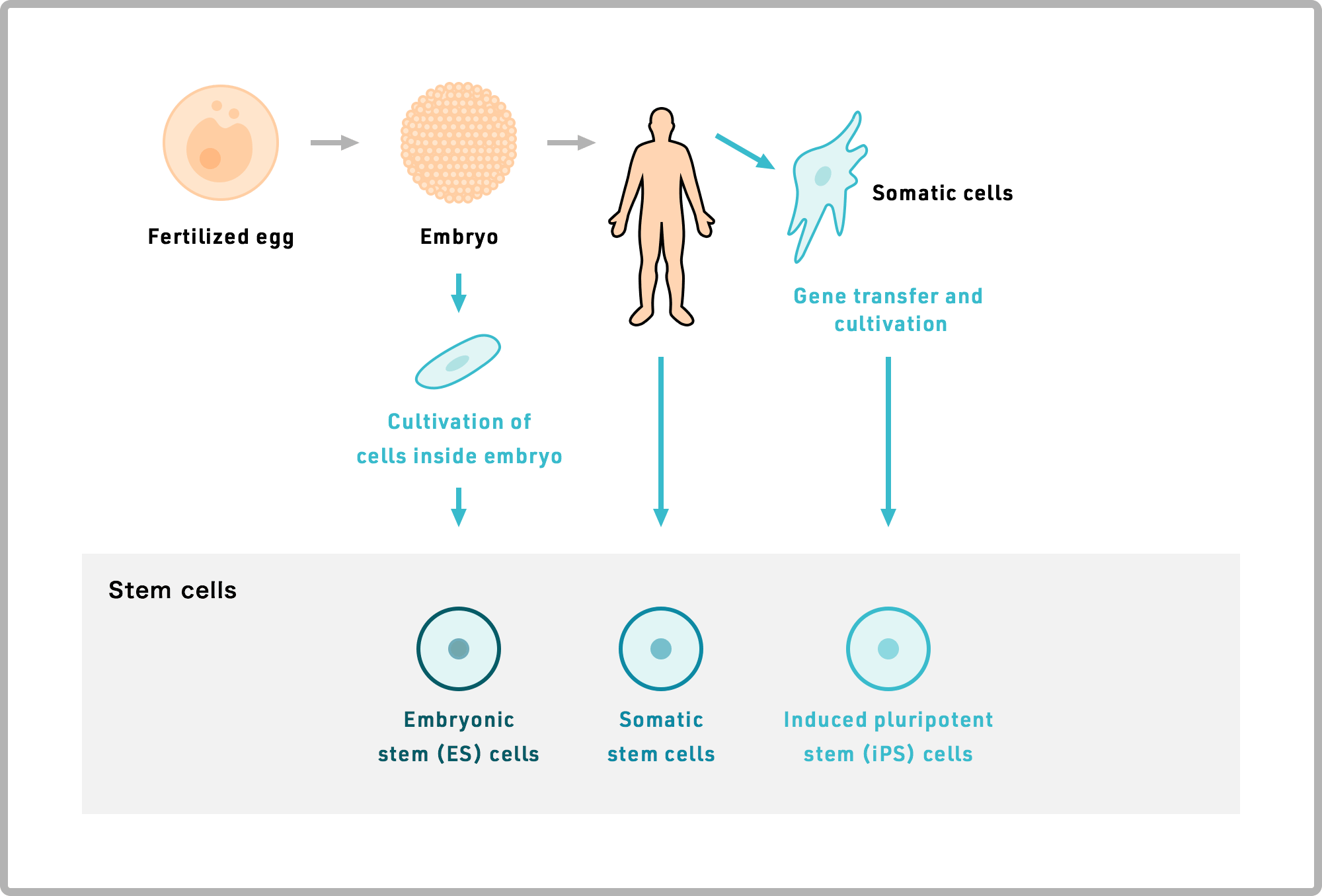
The human body is said to comprise over 37 trillion individual cells belonging to over 200 cell types. Through a repeated process of cell division and proliferation, what starts out as a single fertilized egg ultimately differentiates into the full range of cells that make up the human body (such as nerve cells, cardiac muscle cells, and liver cells).
The human body is made up of both differentiated cells (somatic cells) and cells that are still differentiating (somatic stem cells). Stem cells are characterized by the capacity to self-renew or differentiate into cells that form specific tissues and organs. Somatic stem cells include hematopoietic stem cells, neural stem cells, and mesenchymal stem cells, which differentiate into a limited range of cells. For example, hematopoietic stem cells, found in large numbers in bone marrow, produce hematopoietic cells such as white blood cells and platelets, but they normally do not differentiate into other cell types.
Embryonic stem (ES) cells can differentiate into a much wider variety of cell types than somatic stem cells. They are believed to have the capacity (at least in theory) to develop into the full range of cells that make up the human body, including cardiac muscle cells, nerve cells, liver cells, and blood cells. However, because ES cells are derived from fertilized eggs—in many cases from surplus embryos discarded in infertility treatments—the practice of using such cells for regenerative medicine has stirred debate centered on ethical concerns in many countries. In particular, the use of cells derived from aborted fetuses has drawn wide criticism on ethical grounds.
In 2007, Professor Shinya Yamanaka of Kyoto University successfully developed induced pluripotent stem (iPS) cells—a new form of pluripotent cells that is not derived from fertilized eggs—from human skill cells. iPS cells closely resemble ES cells by virtue of their capacity to differentiate into a wide range of cells, including cardiac muscle cells, nerve cells, liver cells, and blood cells. They offer an advantage over ES cells because they eliminate the ethical concerns. However, iPS cells, like ES cells, can proliferate indefinitely, and issues such as controlling their proliferation capacity will need to be resolved before they can be used in practical applications. iPS cells are an incredible technology with tremendous potential, but it will take some time before they can be put into practical applications.
Regenerative medicine that uses somatic cells (differentiated cells) can only target a limited range of conditions, and development efforts in this field have therefore already reached a mature stage. In contrast, stem cells (which can differentiate into other cells) can be used to target a much broader range of conditions, and are therefore actively being researched around the world.
Among somatic cells, mesenchymal stem cells (MSC), which can be readily isolated and expanded from bone marrow aspirate, are a suitable cell source for regenerative medicine, and they are already used in therapeutic applications.
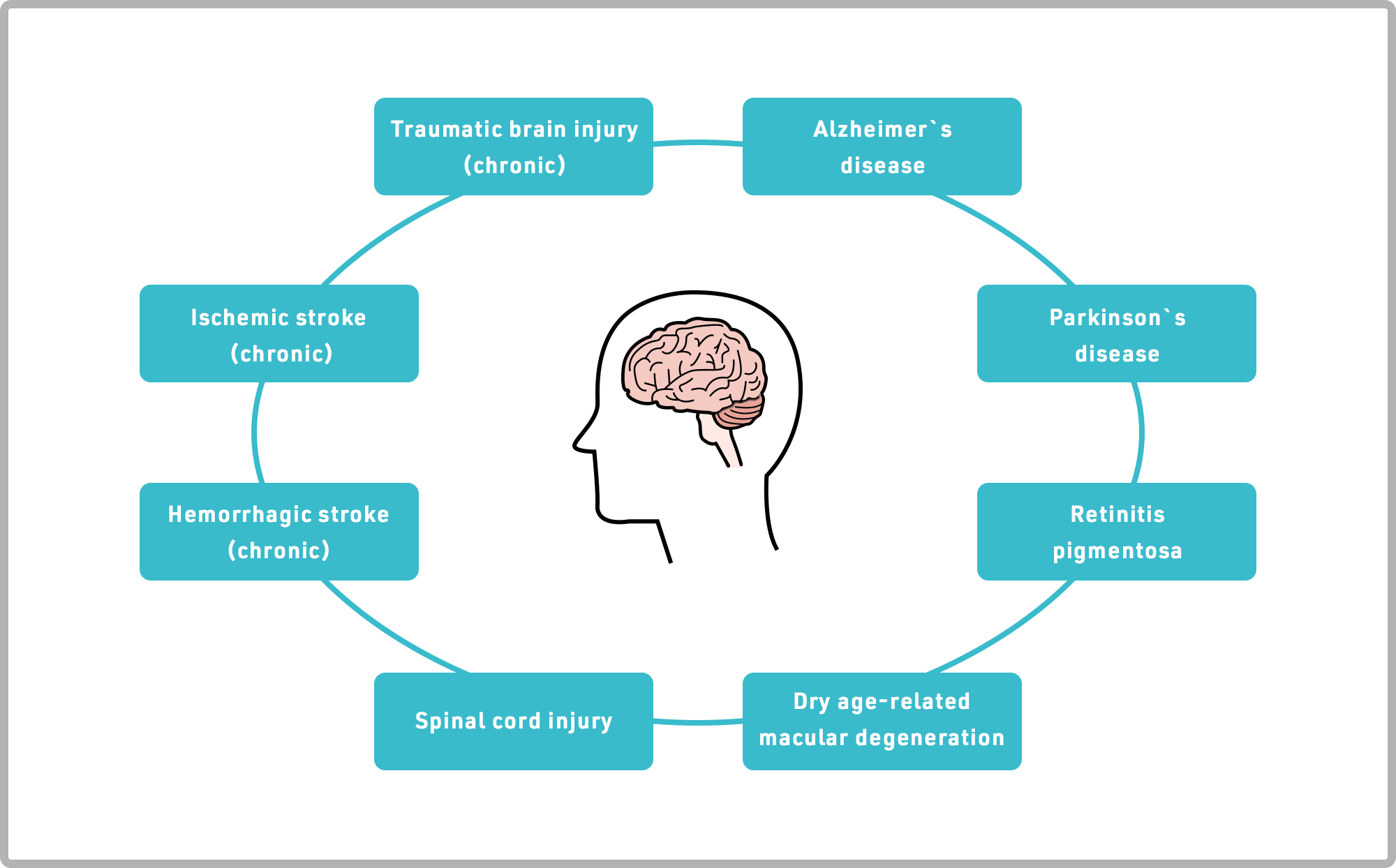
Among regenerative medicines, SanBio focuses on developing products for the central nervous system that are not effectively treated at the present time. Examples of these diseases include dysfunction associated with: stroke, traumatic brain injury, retinal degeneration (e.g., age-related macular degeneration), spinal cord injury, Parkinson’s disease, Alzheimer’s disease, and others.
Our major pipeline SB623 are intended to restore motor and sensory functions by inducing or promoting the innate, natural regenerative processes of patients’ physical functions that were lost due to diseases or accidents.